How to Strenghten Healthcare Systems in the face of Environmental Challenges?
Dr.Goerner and her PH-lab Scientists will use the Science of Flow networks to develop quantitative measures of systemic health goals, which allow practitioners, policy makers and enterprise leaders to track the direction and level of impact of their efforts toward systemic Public health vitality.
This approach to quantitative measures is just as groundbreaking as the regenerative framework itself. We are not simply creating more ways to assess desirable outcomes; we are developing ways to measure the health of the (Health-care) system itself by assessing the causal factors, which support a system’s ability to remain vibrant for long periods of time. Just as elements of circulation, structure, internal and external relationships are critical to human health, so factors such as resilience, efficiency, circulation, structure, relationships, values, and adaptability make or break systemic health of societies and economies.
Just as assessing human health requires measuring multiple factors such as blood pressure and glucose levels, so combining multiple factors of environmental health gives us a clearer picture of how to develop health cares systems that can live long and prosper both internally, and in relationship with the other nested subsystems – social, economic, financial, political– in which they are embedded. The underlying premise is that healthy human systems, ones designed to obey the long-term laws of health, naturally become oriented towards the socially, economically, and environmentally desirable outcomes we currently measure.
A flow-network is any system whose existence arises from and depends on the circulation of critical resources throughout the entirety of their being. Living organisms depend on the circulation of nutrients and oxygen. Ecosystems depend on the circulation of carbon, oxygen, water, etc. health care systems depend on the circulation of money, resources, goods and information. While ecological flow-networks are particularly advanced, the advantage of applying the broader-case principles to public health is that avoids the question of whether the results are merely a metaphoric extrapolation from ecosystems.
We are committed to improving and assessing health outcomes and processes with a specific emphasis on evaluating the effectiveness of evidence based approaches through a comparative regional case study approach. in order to improve system level healthcare delivery, we span our research in key priority healthcare contexts and examine the interrelated complex socio economic forces which can impact the physical and mental well-being of disadvantaged populations. Additionally, our research will examine multiple strands of healthcare delivery including the assurance of reliable health record-based data, clinical performance assessment measures, quality of primary care services and the role of education in improving clinical practices.
'The need to find solutions too many of the world’s health challenges continually increases. The task ahead for the Global Health community worldwide is to reframe and rethink intractable problems based on a range of “unexpected” evidence emerging both locally and globally.'
Please click here for Global Health Policy Blog
Through various partnerships, Planetary Health Lab will facilitate the creation of a healthcare network support by a bedrock of interdisciplinary scientists in order to design the policy and processes that can help design, implement and curie innovative solutions with long positive lasting environmental impact. As a lab we are dedicated to the planetary health, promotion, protection, advocacy and education.
Our Approach:
Our overall goal is to change the trajectories of vulnerable members of the populace, through examining the psychosocial, ecological and biological determinants of health. Our focus will be to build systemic, strategic and effective intervention that address political, social and economic disparities and their associated health outcomes. Psychological, biological, social and environmental processes are all casually related and interact over time to influence health outcomes and exposure to diseases. Our research will explore the links between environmental health factors and social inequalities in health care.
-
To co- design community based participatory research projects on environmental health intervention designed to address access to, nutritious food, clean water, hygiene and sanitation.
-
To design initiatives in the area of performance management, hospital efficiency, quality, continual care and delivery of technological innovations.
-
To apply organizational theory to healthcare with an emphasis on m-health and human centered design in public health.
-
To develop organizational correlates of health and mental service systems.
We are committed to improving and assessing health outcomes and processes with a specific emphasis on evaluating the effectiveness of evidence based approaches through a comparative regional case study approach. In order to improve system level healthcare delivery, we span our research in key priority healthcare contexts and examine the interrelated complex socio economic forces that can impact the physical and mental well being of disadvantaged populations. Additionally, our research will examine multiple strands of healthcare delivery including the assurance of reliable health record-based data, clinical performance assessment measures, quality of primary care services and the role of education in improving clinical practices.
Our Questions:
Q. Is the delivery of healthcare goods engendering some of the rhetoric within the planetary health paradigm?
Q. What are the social, institutional and organization barriers that prevents the co-creation and co-implementation of sustainable practices with the delivery of affordable and quality healthcare?
Q. How can the public and social infrastructure be strengthened to mitigate external shocks that have political, social and economic determinants?
Q. How can we strengthen primary care services to alleviate the burden of (OFF) territory hospitals?
 Exposure Assessment and Control
Exposure Assessment and Control
A Network Theory Approach to Healthcare System Strengthening
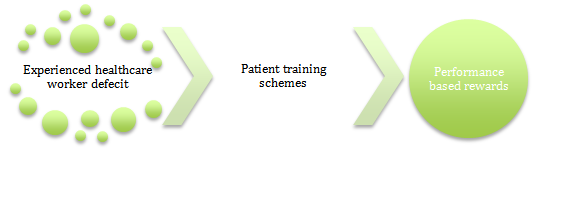
Planetary Health Lab is focusing on building an ambitious project to train community health workers via e-health tools to develop the procedural expertise and techniques needed for public health care delivery. In order to build a community based health workforce, training will take place to manage the bio-psychosocial factors underpinning NCDs; whereas the greater burden of delivering care for challenging clinical conditions will be addressed through enhanced surgical training and mentorship programs for emergency medicines practices.
Aims:
-
To build context specific solutions with the ministry of health through the careful pooling of financial resources and the strategic deployments of experienced healthcare workers running training workshops.
-
To create a collaborative learning environment that relies on the interexchange of researchers to deliver key environmental healthcare programs that warrant a context specific solution i.e. Family planning programs.
-
To create sustainable technological solutions to complex challenges such as waste disposal, clean water and by fostering public-private partnerships.
-
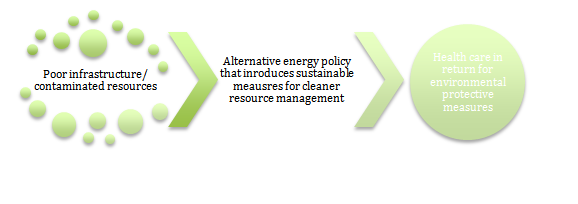
To augment a smart new energy policy that assesses the benefits of solar panel technology and bio clean water filters.
-
To measure environmental indices so as to systemically uncover the interplay of these with other determinants of health and disease
-
To incorporate sustainable farming practices to tackle high rates of nutritional deficiency within Maternal-child health Programs.
-
To devise monitoring schemes to achieve quantitative goals that demonstrates the effectiveness of interventions.
Our Processes:
Mental Health Projects
According to WHO, mental health will cost economies $16 trillion by 2030, and by 2020, depression will be the second greatest contributor to the global burden of disease. The OECD estimates that mental illnesses will cost European economies 3% of their GDP. Increasingly, mental health is seen as falling into the realm of environmental health, however whilst environmentally induced infectious diseases have their associated risk factors mapped out, such as sanitary conditions and mal nourishment, mental health has yet to map out such measures. If risk factors are mapped out between mental health and the physical environment, this could lead to preventive measures being identified and put in place to reduce mortality and morbidity associated with mental health. The slower progress on mental health is in part due to the complex interaction of genes and the environment; for instance, research published by Dr David St Clair within the Journal of the American Medical Association (JAMA) found compelling evidence suggesting a link between famines induced maternal starvation in pregnancy leading to the onset of schizophrenia within children. Similar research by Dr Jianghong Liu at Penn State University demonstrates the impact of nutritional deficiencies causing an epigenetic effect on genes required for brain development. This is more worrying when we consider the potential effect on crop yields of rising temperatures and varying humidity and rainfall given climate change.
We propose that if these complex and syndromic risk factors are mapped out between mental health and the physical environment, this could lead to preventive measures being identified and put in place to reduce mortality and morbidity associated with mental health.
We recognise that the slower progress on mental health is in part due to the complex interaction of genes and environment. However emerging data is pointing towards a critical juncture.
‘The impact of climate change is a breeding ground for psychopathology’ Lisa Vas Strassen
There is increasing research that suggests that both emotional well-being, and, at the other end of the spectrum, brain disorders, are intertwined with a set of complex cognitive, emotional and social- environmental factors. At the same time, philosophers have suggested a relationship between the human mind and the physical environment across millennia implying a multifaceted relationship between the human mind and our environment. Applying complex systems thinking suggests that a multidisciplinary approach is warranted to better understand this relationship and the existing systems that underpins it, including the underlying incentives that drive the overall system. Taking such an approach will also allow us to understand better the blockages in the complex system that need to be addressed to allow better data collection, information flow, and the development of additional technological solutions to address mental health challenges and to enhance emotional well-being.
Ecomindbot
Ecomindbot will contribute to the growing effort of research that explores approaches in evaluating the psychological impacts of nature, as well as help strengthen the scientific case for ecosystem services as a healthcare interventionist strategy through the digitization of eco-therapy.
Broadly speaking, ECOMINDBOT has its scientific basis on the following pre-existing theoretical frameworks:
-
Free-Energy Principle/ Consciousness.
-
Embodied Cognition and Extended Mind Theory.
-
Gibson’s Theory of Perception.
-
Emotional regulation and psychological Well-being.
Our Collaborations are based on the following objectives:
-
To build technological collaborations that help forge cooperation between environmental epidemiologists, biomedical engineers and environmental scientists.
-
To ensure the continuation of any pre-existing environmental programs and solutions through training and building of local capacity to maintain & implement environmental sustainable practices.
-
To utilise the indispensible local knowledge of NGOs so as to monitor and measure the impact of implementing environmentally sustainable efforts, which have a positive, long-term effect in the community.
-
To collaborate and design joint environmental monitoring strategies that helps assess environmental outcomes and impacts; PH-lab would then like to draw on results of monitoring practices to design new follow up sustainable projects.
-
To collaborate with current and emergent efforts to learn and catalyse greater alignment between market forces and planetary health improvements.